Migraine has also been referred to as a neurovascular headache due to the fact that one aspect of migraine development involves changes in the chemistry and diameter of the blood vessels that provides blood to the brain and the nerves in the neck and head.
A migraine can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It’s often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last for hours to days, and the pain can be so severe that it interferes with your daily activities.
For some people, a warning symptom known as an aura occurs before or with the headache. An aura can include visual disturbances, such as flashes of light or blind spots, or other disturbances, such as tingling on one side of the face or in an arm or leg and difficulty speaking.
Medications can help prevent some migraines and make them less painful. The right medicines, combined with self-help remedies and lifestyle changes, might help.

What causes migraines?
Researchers believe that migraine has a genetic cause. There are also a number of factors that can trigger a migraine. These factors vary from person to person, and they include
- Stress
- Anxiety
- Hormonal changes in women
- Bright or flashing lights
- Loud noises
- Strong smells
- Medicines
- Too much or not enough sleep
- Sudden changes in weather or environment
- Overexertion (too much physical activity)
- Tobacco
- Caffeine or caffeine withdrawal
- Skipped meals
- Medication overuse (taking medicine for migraines too often)
Some people have found that certain foods or ingredients can trigger headaches, especially when they are combined with other triggers. These foods and ingredients include
- Alcohol
- Chocolate
- Aged cheeses
- Monosodium glutamate (MSG)
- Some fruits and nuts
- Fermented or pickled goods
- Yeast
- Cured or processed meats
Symptoms
Migraines, which often begin in childhood, adolescence or early adulthood, can progress through four stages: prodrome, aura, attack and post-drome. Not everyone who has migraines goes through all stages.
Prodrome
One or two days before a migraine, you might notice subtle changes that warn of an upcoming migraine, including:
- Constipation
- Mood changes, from depression to euphoria
- Food cravings
- Neck stiffness
- Increased thirst and urination
- Frequent yawning
Aura
For some people, aura might occur before or during migraines. Auras are reversible symptoms of the nervous system. They’re usually visual, but can also include other disturbances. Each symptom usually begins gradually, builds up over several minutes and lasts for 20 to 60 minutes.
Examples of migraine aura include:
- Visual phenomena, such as seeing various shapes, bright spots or flashes of light
- Vision loss
- Pins and needles sensations in an arm or leg
- Weakness or numbness in the face or one side of the body
- Difficulty speaking
- Hearing noises or music
- Uncontrollable jerking or other movements
Attack
A migraine usually lasts from four to 72 hours if untreated. How often migraines occur varies from person to person. Migraines might occur rarely or strike several times a month.
During a migraine, you might have:
- Pain usually on one side of your head, but often on both sides
- Pain that throbs or pulses
- Sensitivity to light, sound, and sometimes smell and touch
- Nausea and vomiting
Post-drome
After a migraine attack, you might feel drained, confused and washed out for up to a day. Some people report feeling elated. Sudden head movement might bring on the pain again briefly.
Migraine Risk factors
Several factors make you more prone to having migraines, including:
- Family history. If you have a family member with migraines, then you have a good chance of developing them too.
- Age. Migraines can begin at any age, though the first often occurs during adolescence. Migraines tend to peak during your 30s, and gradually become less severe and less frequent in the following decades.
- Sex. Women are three times more likely to have migraines.
- Hormonal changes. For women who have migraines, headaches might begin just before or shortly after onset of menstruation. They might also change during pregnancy or menopause. Migraines generally improve after menopause.
The common belief is that the sequence of occurrence of the migraine headache pains is as follows:
1 . First the blood vessels surrounding the brain becomes dilated and starting pressing on the adjacent nerves. It is still a mystery though on exactly how and why these blood vessels dilate although it seems that there is some form of chemical signal that is activating the pain sensors in the trigeminal nerve that runs from a location near the skull center, up and over the eyes and then towards the forehead.
2 . These stimulated nerve fibers then release fragments of proteins, known as neuropeptides, which cause the swelling and inflammation of the blood vessels.
3. The expansion of the blood vessels irritates the trigeminal nerve further, like a vicious cycle, resulting in the migraine headache pain.
|
FIORICET® with CODEINE (Fee-OR-a-cet) (Butalbital, Acetaminophen, Caffeine, and Codeine Phosphate) capsules, CIII |
|
FIORICET with CODEINE is:
|
|
Important information about FIORICET with CODEINE:
|
|
Important Information Guiding Use in Pediatric Patients:
|
|
Do not take FIORICET with CODEINE if you have:
|
|
Before taking FIORICET with CODEINE, tell your healthcare provider if you have a history of:
|
|
Tell your healthcare provider if you are:
|
|
When taking FIORICET with CODEINE:
|
|
While taking FIORICET with CODEINE DO NOT:
|
|
The possible side effects of FIORICET with CODEINE:
Get emergency medical help if you:
These are not all the possible side effects of FIORICET with CODEINE. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to dailymed.nlm.nih.gov Manufactured by: Nexgen Pharma, Inc., Irvine, CA 92606 Distributed By: Actavis Pharma, Inc., Parsippany, NJ 07054 USA |
Symptoms of migraine
A migraine attack typically goes through four distinct phases where the migraine sufferers will encounter certain migraine symptoms for each phase.
Prodrome phase
General symptoms experienced in the prodrome phase, also known as the preheadache phase, includes irritability, increased yawning, fatigue, mood swings and food cravings.
Aura phase
About 15% of migraine sufferers can experience an aura before the development of the migraine headache. Symptoms experienced are weakness or numbness on one side of the body, visual disturbances such as seeing blind spots and flashing lights, slurred speech and sensitivity to sound and light.
Headache phase
The migraine headache phase can usually last between 4 to 72 hours and is considered to be the most scary and painful phase. The symptom encountered is a throbbing headache where in about 60% of the cases, the headache occurs on only one side of the head. Other associated symptoms experienced includes diarrhea, nausea and vomiting, dizziness, lightheadedness and tinnitus.
Postdrome phase
The postdrome phase is when the pain and other associated symptoms have resolved and most of the time the migraine sufferer just feel like wanting to be left alone. Common symptoms encountered in this phase are surge in energy, increased appetite, euphoria, fatigue and confusion.
Not all migraine sufferers will go through all the four phases though. An example is a person who is suffering from migraine without aura, will completely skip the aura phase during the migraine attack. It is important that we understand what is migraine and the symptoms of migraine indepth so that we can differentiate it from other types of headaches and be able to seek appropriate treatment.
Migraine Causes
Though migraine causes aren’t fully understood, genetics and environmental factors appear to play a role.
Changes in the brainstem and its interactions with the trigeminal nerve, a major pain pathway, might be involved. So might imbalances in brain chemicals — including serotonin, which helps regulate pain in your nervous system.
Researchers are studying the role of serotonin in migraines. Other neurotransmitters play a role in the pain of migraine, including calcitonin gene-related peptide (CGRP).
What is the best medicine for migraine?
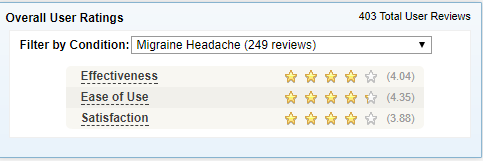
Fioricet is the best medicine for migraine and almost 80% patient likes to treat migraine using fioricet.
Fiorinal and Fioricet are medicines for tension-type headaches. Fiorinal contains aspirin and Fioricet contains acetaminophen. They both contain butalbital and caffeine. Codeine is sometimes also added to this combination. Butalbital, a barbiturate sedative, is habit-forming.
These medications should not be used on a daily basis because dependency on them can develop. Regular use, more than 2 days per week, can cause rebound headache, which may not respond to usually effective acute and preventive treatments.
